ABOUT OBESITY
We all need food to survive. The need to supply food to generate energy is a driving force in the biology of all living organisms. It is more than natural for our body to have a complex system operated by our hormones in terms of control to nutrient intake.
CAUSES OF OBESITY
Obesity may be developed secondary due to many biological, psychological and even social reasons. The most important factors are imbalanced high-calorie diet and immobility.
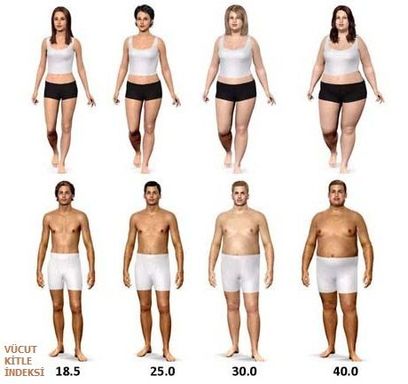
The most preferred method for determining the weight category and the degree of obesity is the calculation of the BODY MASS INDEX (BMI).
BMI is the number estimation of a person`s body weight in kilograms divided by the square of the same person`s height in meters. It is not changeable due to age and gender.
When the excess weight exceeds 25-30 kg (4-5 st) above the certain limits, the case is regarded as “morbid obesity – a type of obesity seen regarded as a serious medical condition. For such patients, the chance of permanent weight loss with diet and exercise therapies is very low. Therefore, surgery is the valid and efficient treatment option for the people with morbid obesity.
Because BMI doesn't reflect;
-age related differences
-sex related differences
-race related differences
BMI doesn’t indicate body fat distribution
BMI isn’t distinctive for determining risks of obesity related diseases
BMI is deceptive for children, pregnant or athletic patients
- 1 / 2
- »